ECMO Treatment
ECMO Treatment in Vadodara | Life-Saving Heart & Lung Support
Extracorporeal Membrane Oxygenation (ECMO) – Advanced Critical Care Support
ECMO treatment in Vadodara represents one of the most advanced life-support technologies used in critical care medicine. ECMO (Extracorporeal Membrane Oxygenation) is designed for patients whose heart and/or lungs are unable to function adequately, even with conventional treatments such as ventilators or medications. It plays a vital role when standard breathing or cardiac support is insufficient, providing external assistance to maintain proper oxygenation and effective carbon dioxide removal from the body.
At Janvi Multispeciality Hospital, Vadodara, our expert critical care team offers ECMO support to patients with severe respiratory or cardiac failure. This advanced therapy allows the heart and lungs to rest and heal while essential life functions continue.
What Is ECMO?
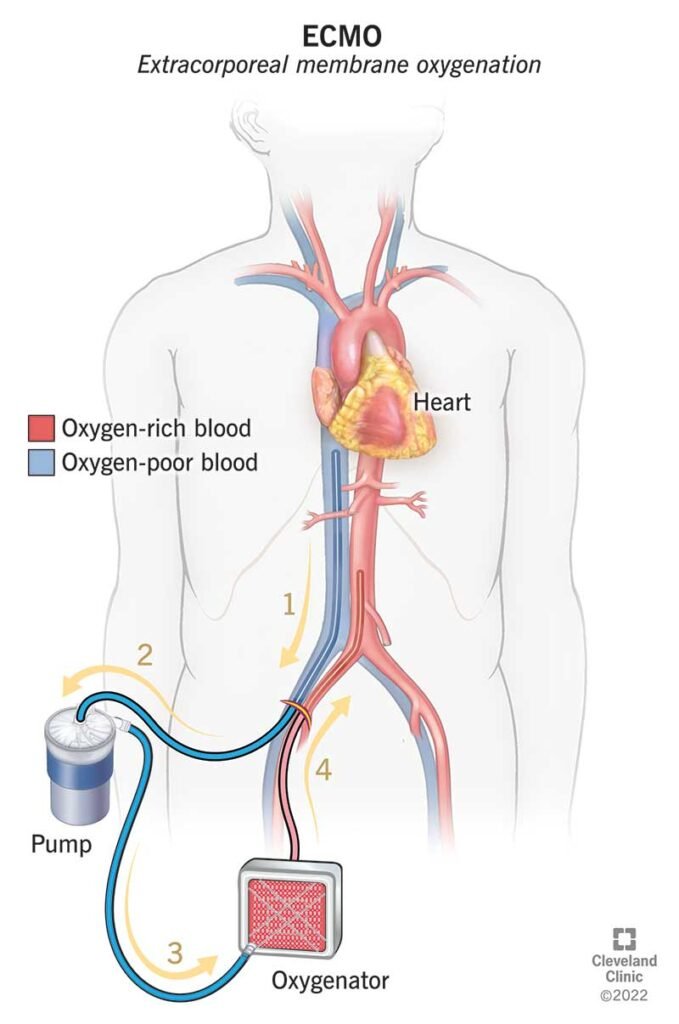
ECMO is a specialized form of artificial life support that temporarily takes over the work of the heart and lungs. During ECMO treatment, blood is continuously circulated outside the body through a machine that:
Adds oxygen to the blood
Removes carbon dioxide
Returns the oxygenated blood back into the body
This process mimics lung function and provides critical oxygen delivery when the patient’s own organs cannot perform adequately.
“Extracorporeal” refers to the process occurring outside the body, and “membrane oxygenation” refers to the exchange of gases — oxygen and carbon dioxide — through a membrane.
Types of ECMO
There are two main types of ECMO, each used for different clinical scenarios:
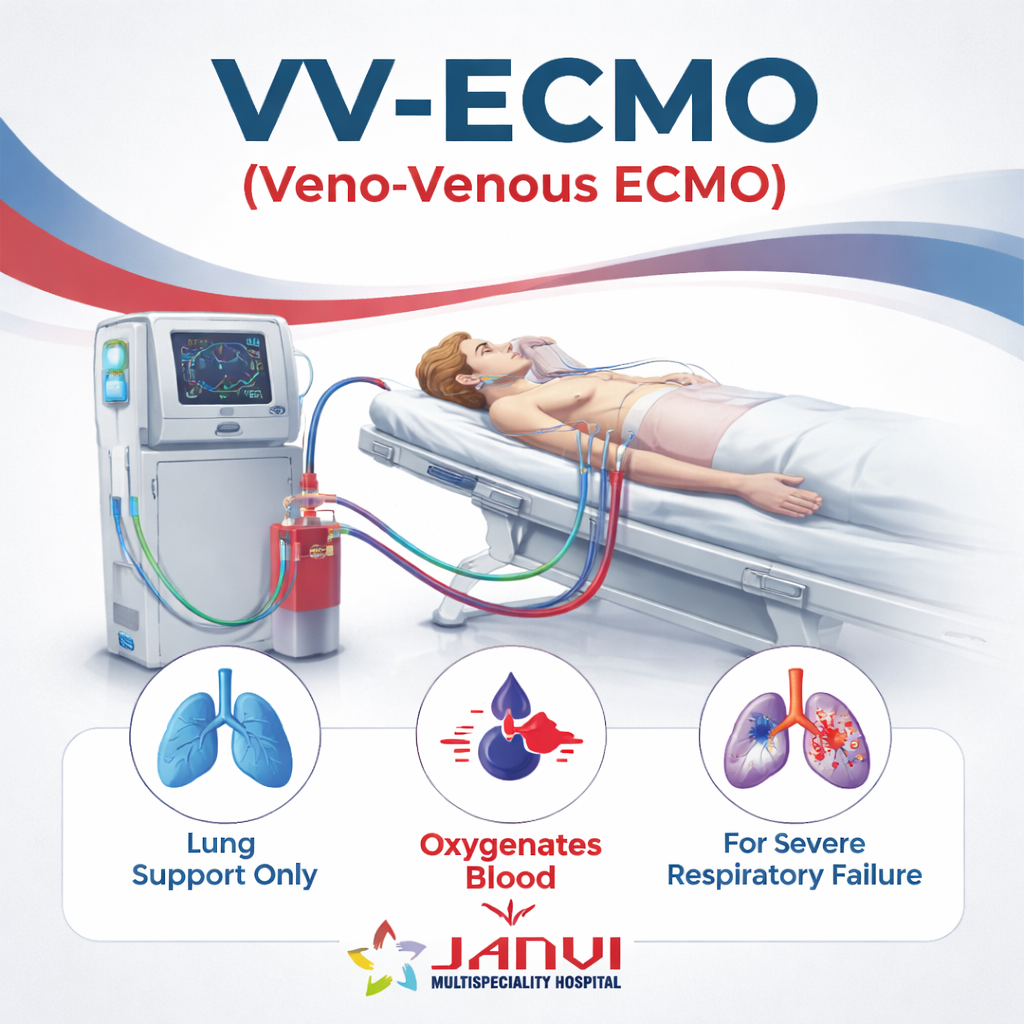
VV-ECMO (Veno-Venous ECMO)
- Provides lung support only
- Supports oxygenation in patients with severe respiratory failure
- Typically used when the heart function is relatively preserved
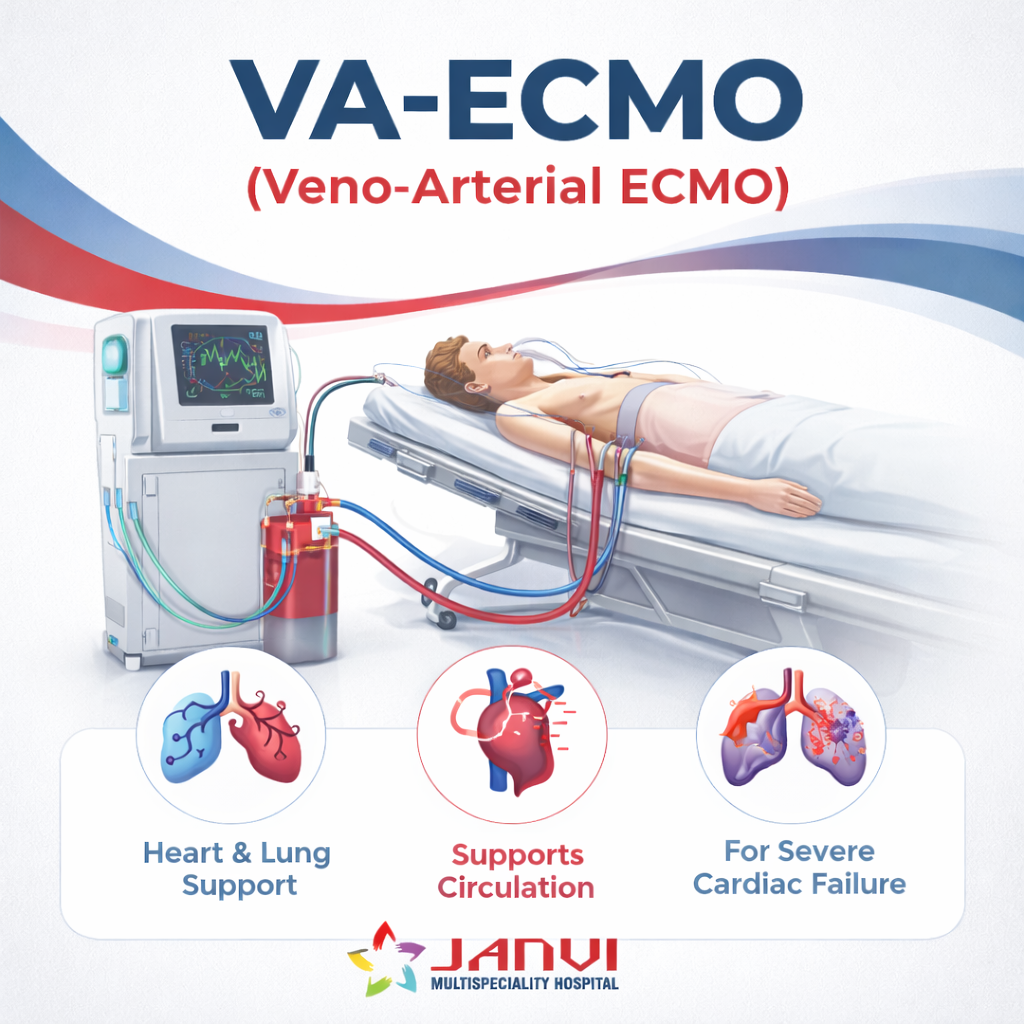
VA-ECMO (Veno-Arterial ECMO)
- Provides both heart and lung support
- Bypasses the heart and lungs to support circulation
- Used in severe cardiac failure, cardiogenic shock, or post-cardiac arrest
Who Needs ECMO?
ECMO may be required in life-threatening conditions when other treatments fail, including:
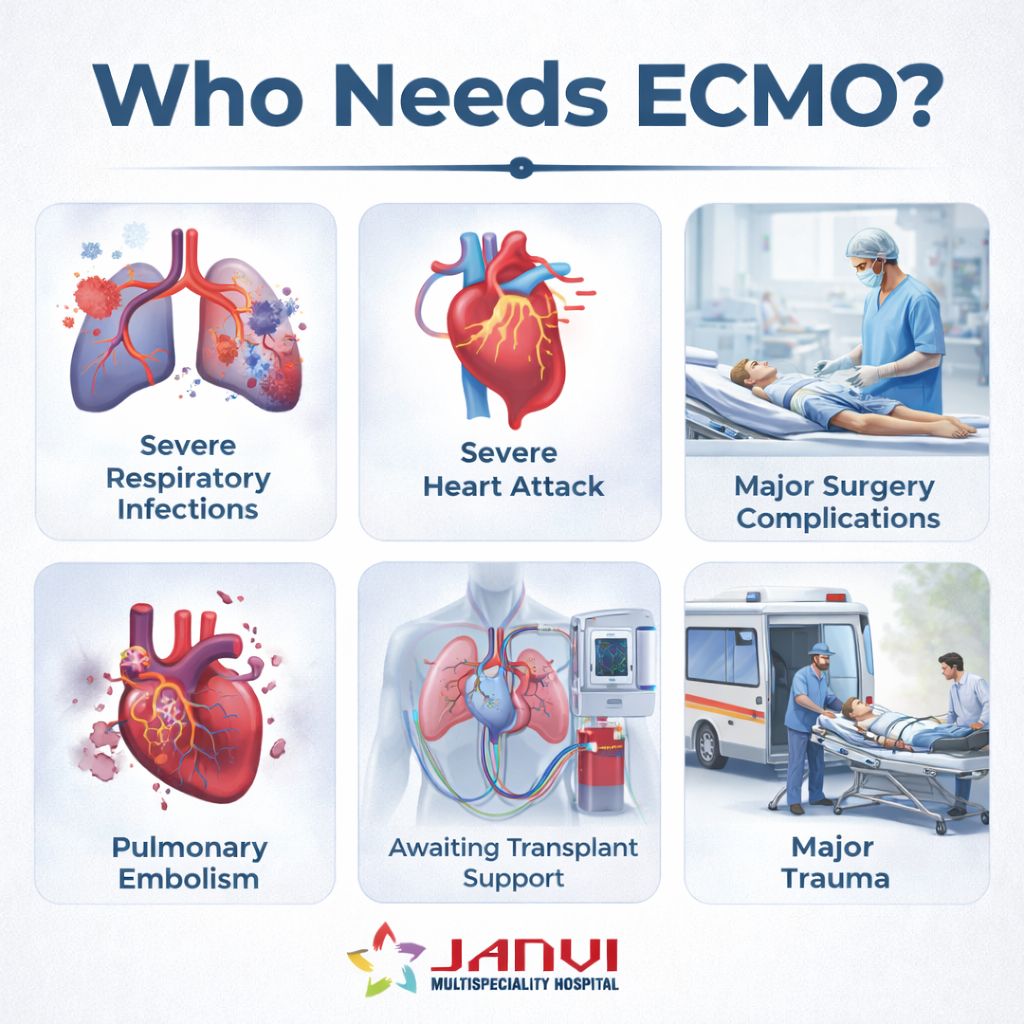
- Acute Respiratory Distress Syndrome (ARDS)
- Severe respiratory infections
- Heart attacks with severe cardiac dysfunction
- Trauma affecting heart or lung function
- Pulmonary embolism
- Complications following major surgery
- Critical cases of COVID-19
- Conditions requiring heart or lung transplant support
- Patients awaiting organ transplant or recovering from transplant
Treatment Details
What happens during an ECMO procedure?
During ECMO, blood flows out of your body through a tube in a large blood vessel in your chest, legs or neck. A pump pushes your blood through tubes that carry it to a machine that adds oxygen and removes carbon dioxide. Then, the ECMO machine pumps your blood back into your body.
A healthcare provider may refer to the process of placing these tubes as ECMO cannulation. You’ll be sedated, so you won’t feel the tubes going in. During extracorporeal membrane oxygenation, you may be awake or sedated.
An ECMO specialist will routinely check your heart and lung functions while you’re on ECMO to make sure you’re in good condition and there are no complications. This also lets providers know how much longer to keep you on ECMO.
Once you show signs of recovery, providers will begin weaning you off ECMO. In most cases, this process takes between two and five days. Then, a provider will remove the tubes and stitch the skin where the tubes were.
How long will I need this treatment?
The length of time you spend on ECMO depends on why you need it. People can stay on extracorporeal membrane oxygenation anywhere from hours to days to weeks. The ECMO machine gives your lungs (and sometimes your heart, too) a chance to rest and recover. Meanwhile, healthcare providers treat the conditions you have.
What are the potential benefits and risks of ECMO?
An ECMO machine can be a lifesaving tool for people who are critically ill. It can support their lungs and heart, which can:
- Ease the strain on your heart and lungs, making it possible for these organs to heal
- Keep you alive during surgery or another medical procedure
- Support you as you wait for a transplant
- Help infants who were born with heart issues or lungs that weren’t fully developed
While an ECMO machine is a vital medical tool, it’s also one that has risks. Some of them are significant. The risks of extracorporeal membrane oxygenation include:
- Clotting problems: Anyone on ECMO also has to be on blood thinners because of the risk of clots forming. Clots could also become stuck in the ECMO circuit, interrupting blood flow.
- Infection: Any break in your skin poses a risk for infection, and the tubes of an ECMO circuit can give an infection direct access to your bloodstream. This can make it easier for an infection to spread throughout your body.
- Bleeding: Because tubes have to go into major arteries and veins, this can increase your risk of bleeding. Blood thinners also increase the risk of bleeding.
- Low or uneven blood oxygen levels: In general, ECMO’s target range is slightly lower than normal blood oxygen levels. Maintaining an even blood oxygen level throughout your body can also be a challenge.
- ECMO circuit failure: A mechanical failure in any part of the ECMO circuit can cause the entire circuit to stop. This can be life-threatening.
- Stroke: Stroke can occur as a result of either sudden bleeding in the brain during ECMO support or from clots in the circuit that end up traveling to the brain. This can be life-threatening.
What is the survival rate on ECMO?
The survival rate varies widely depending on the reason a healthcare provider uses ECMO. For example, anywhere from 4 to 8 out of 10 neonates may survive ECMO. Survival rates for babies with heart failure may be lower than for those with lung issues.
Researchers studying life expectancy after ECMO found that about 3 out of 10 adults lived five years after ECMO. Nearly 8 out of 10 people who survived the first 30 days lived another five years.
Is ECMO a last resort?
Healthcare providers use ECMO for people who have severe heart or lung problems when other treatments have failed. They use this treatment for conditions that can get better. But you can still die while on ECMO if providers can’t fix the condition you have.




